“Those who cannot remember the past are condemned to repeat it”
George Santayana
To look at the History of Medicine is to realise how often diseases recur and, sadly, how humans repeat the same mistakes. It is easy to look back with the benefit of hindsight and with modern medical knowledge but we must remember how we remain as fallible as our forebears.
Our first introduction to the History of Medicine is often through learning about the Black Death at school. The story is very familiar; between 1347 and 1351 plague swept the whole of Europe killing between a third and two-thirds of the continent. At the time it was felt the end of the world was coming as a disease never before seen took up to 200 million lives. However, this was actually the second time plague had hit Europe. Nearly a thousand years earlier the first plague pandemic had devastated parts of Europe and the Mediterranean. Half the population of Europe were affected. This was Justinian’s plague, named for the Holy Roman Emperor whose reign the disease helped to define. Yet despite the carnage Europe forgot and had no preparation when plague returned.
Between 2014 and 2016 nearly 30,000 people were hit by the Ebola outbreak in West Africa. Our systems were found lacking as the disease struck in a way never before seen. We said we would learn from our mistakes. Never again.
Yet the current Ebola epidemic in the Democratic Republic of the Congo (DRC) is proving that even today it is hard to remember the lessons of the past and how disease will find any hole in our memory. This is the story of Justinian’s plague, the lessons we failed to learn then and now as we struggle with Ebola.
Justinian’s Plague
Justinian I. Contemporary portrait in the Basilica of San Vitale, Ravenna . From Wikipedia.
It’s 542 CE in Constantinople (now Istanbul). A century earlier the Western provinces of the Roman Empire collapsed. The Eastern empire continues in what will be called the Eastern Roman or Byzantine Empire. Constantinople is the capital city, then as now, a melting pot between Europe and Asia. Since 527 CE this Empire has been ruled by Justian I, an absolute monarch determined to return to the glory years of conquest.
The Empire has already expanded to cover swathes of Northern Africa. Justinian’s focus is now on reclaiming Italy. The Empire is confident and proud, a jewel in an otherwise divided Europe now in the Dark Ages.
The Eastern Roman Empire at the succession of Justinian I (purple) in 527 CE and the lands conquered by the end of his reign in 565 CE (yellow). From US Military Academy.
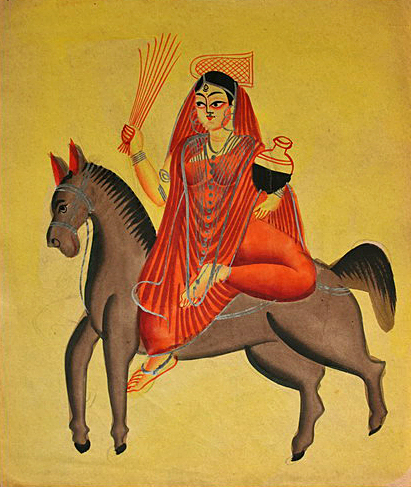
Procopius of Caesarea (Creative Commons)
The main contemporary chronicler of the plague of Justinian, Procopius of Caesarea (500-565 CE) identified the plague as arriving in Egypt on the Nile’s north and east shores. From there it spread to Alexandria in the north of Egypt and east to Palestine. The Nile was a major route of trade from the great lakes of Africa to the south. We now know that black rats on board trade ships brought the plague initially from China and India via Africa and the Nile to Justinian’s Empire.
Procopius noted that there had been a particularly long period of cold weather in Southern Italy causing famine and migration throughout the Empire. Perfect conditions to help a disease spread.
In his book Secret History Procopius detailed the symptoms of this new plague: delusions, nightmares, fevers and swellings in the groin, armpits, and behind their ears. For most came an agonising death. Procopius was of no doubt that this was God’s vengeance against Justinian, a man he claimed was supernatural and demonic.
Justinian’s war in Italy helped spread disease but so did peace in the areas he’d conquered. The established trade routes in Northern Africa and Eastern Europe, with Constantinople in the centre, formed a network of contagion. Plague swept throughout the Mediterranean. Constantinople was under siege for four months during which time Procopius alleged 10,000 people died a day in the city. Modern historians believe this figure to be closer to a still incredible 5,000 a day. Corpses littered the city streets. In scenes prescient of the Black Death, mass plague pits were dug with bodies thrown in and piled on top of each other. Other victims were disposed of at sea. Justinian was struck down but survived. Others in Constantinople were not so lucky, in just four months up to 40% of its citizens died.
The plague’s legacy
The plague continued to weaken the Empire, making it harder to defend. Like the medieval kings after him Justinian I struggled to maintain the status quo and tried to impose the same levels of taxation and expansion. He died in 565 CE. His obsession with empire building has led to his legacy as the ‘last Roman’. By the end of the sixth century much of the land in Italy Justinian had conquered had been lost but the Empire had pushed east into Persia. Far from Constantinople the plague continued in the countryside. The plague finally vanished in 750 CE by which point up to 50 million people had died, 25% of the population of the Empire.
Procopius’s description of the Justinian plague sounds like a lot like bubonic plague. This suspicion was confirmed in recent research.
Yersinia pestis bacteria, Creative Commons
At a two separate graves in Bavaria bacterial DNA was extracted from the remains of Justinian plague victims. The DNA matched that of Yersinia pestis the bacterium which causes bubonic plague. The DNA was analysed and found to be most closely related with Y. pestis still endemic to this day in Central Asia. This suggests the route from infection via trade from Asia to Europe.
After 750 CE plague vanished from Europe. New conquerors came and went with the end of the Dark Ages and the rise of the Middle Ages. Europeans forgot about plague. In 1347 they would get a very nasty reminder.
It’s very easy now in our halcyon era of medical advances to feel somewhat smug. Yes, an interesting story but wouldn’t happen now. Medieval scholars didn’t have germ theory. Or a way of easy accessing Procopius’s work. Things are different now.
We’d study Justinian’s plague with its high mortality. We’d identify the cause. We’d work backwards and spot how the trade link with Asia was the route of infection. We’d work to identify potential outbreaks in their early stages in Asia. By the time the second plague epidemic was just starting we’d notice it. There would be warnings to spot disease in travelers and protocols for dealing with mass casualties and disposal of bodies. We’d initiate rapid treatment and vaccination if possible. We’d be OK.
Ebola shows how hard this supposedly simple process remains.
Ebola: A Modern Plague
The Ebola virus (Creative Commons)
Ebola Viral Disease is a type of viral haemorrhagic fever first identified in 1976 during an outbreak in what is now South Sudan and the DRC. Caused a spaghetti-like virus known as a filovirus this disease causes severe dehydration through vomiting and diarrhoea before internal and external bleeding can develop. Named for the Ebola River where it was first identified it spreads by direct human contact with a mortality rate varying from 25% to 90%. An epidemic has been ongoing in DRC since August 2018. We are in our fourth decade of knowing about Ebola. And five years ago we were given the biggest warning yet about its danger.
Up until 2014 the largest outbreak of Ebola had affected 315 people. Other outbreaks were much smaller. Ebola seemed to burn brightly but with only a few embers. In 2014 it became a forest fire.
A healthcare worker during the Ebola outbreak of 2014-16 (From CNN.com)
The West Africa Epidemic of 2014-16 hit Guinea, Sierra Leone and Liberia. The disease showed its potential in our age of global travel as the first cases appeared in America and Europe. In all there were 28,160 reported cases. 11,308 people died. Ebola caught the world napping. What had been a rare disease of Africa was potentially a threat to us all. Suspicion of foreign healthcare workers and miscommunication about the causes of Ebola were blamed for helping to further the disease. Yet there was hope as promising experimental vaccines were put into production.
As the forest fire finally died down there was a chance to reflect. There were many publications, including from Médecins sans frontières, about the lessons learnt from Ebola and how not to repeat the lessons from the past. These were all along similar themes: the importance of trained frontline staff, rapid identification of the disease, engaging and informing local communities, employing simple yet effective methods to provide disease spread and the use of the new vaccine to protect contacts and contacts of contacts. There was lots of criticism about the speed of the World Health Organisation response but also a feeling that with new tools and lessons learnt things would be different next time.
When Ebola surfaced again last year in the DRC there was initial hope that lessons were learnt. Over 100,000 people have been vaccinated; a new weapon. However, the disease continues a year on with over 1000 cases and over 800 fatalities and fresh concern that this outbreak is far from over.
There remains delays in identifying patients with Ebola; not surprising as the early symptoms mimic more common diseases such as malaria. As a result patients are not isolated quickly enough and may infect others before their test results are back. Also the talk of engaging communities is falling flat. In a region torn apart by decades of civil unrest there is widespread mistrust of authorities with blame falling on the Ebola units themselves for causing death. It is estimated that 30% of patients are staying at home and being a potent vector for disease rather than coming forward. There has also been violence against healthcare workers and hospitals as a result of this fear. Reassuringly, where local communities and healthcare has come together Ebola has been stopped but this is not the norm and behavioural scientists are being used to help connect with locals. Despite the lessons learnt Ebola is continuing to be a difficult adversary.
It is easy in the West to feel we are immune from misinformation and fear. Yet look at the current measles epidemic in New York State. Look at the anti-vaccination movement, labelled a “public health timebomb” by Simon Stevens, the chief executive of NHS England last week. We are no more immune than anyone else to irrationality. Nor too proud to learn the lessons of the past; the ‘ring’ style of vaccinating contacts against Ebola is the same as used during the successful campaign to eradicate smallpox over four decades ago.
Medical advances have come on in ways no-one in the Middle Ages could have foreseen. We have never had more ways to share our knowledge of disease or so many ways to prevent suffering. Yet people remain the same. And that’s the tricky part. Let’s not forget that bit.
Thanks for reading
- Jamie